
Corneal collagen cross-linking is a technique that was first used in 1998 to treat patients with a disease called keratoconus. In keratoconus, the cornea (the front clear window of the eye) can become weak, thin, and irregularly shaped.
Instead of keeping its normal round shape, corneas with keratoconus can bulge forward into the shape of a cone causing poor vision. We began treating patients with CXL as part of a clinical study several years prior to the procedure’s approval by the FDA.
CXL is now being routinely performed for patients with keratoconus as a way to strengthen the cornea slow the progression of the disease.
What is keratoconus?
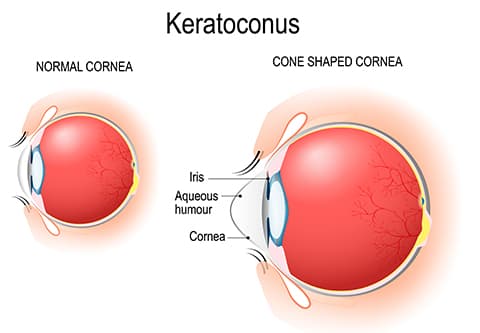
Keratoconus is a common disease that occurs in approximately 1 in 750 Americans. In this condition, the cornea becomes weak, progressively thinner, and irregular in shape which can cause high levels of astigmatism.
Instead of a normal, relatively round shape resulting in clear vision, the cornea in keratoconus can become cone-shaped. This can interfere with the ability to see clearly. Often keratoconus patients first require glasses, then contact lenses, and, if the condition progresses to a severe level, a corneal transplant may be required.
What is astigmatism?
Astigmatism means that the front surface of the eye (the cornea or clear window in front of the eye) is less round and more irregular in shape so the image won’t focus clearly on the retina in the back of the eye. This can result in poor vision and glare.
Most patients with astigmatism can be nicely treated with glasses, contact lenses, LASIK, or toric lens implants. However, keratoconus eyes develop a type of astigmatism called “irregular astigmatism,” causing distorted vision that may not be nicely correctable with conventional modalities.
What does CXL do?
Normal corneas have crosslinks between its collagen fibers that keep it strong and able to retain its normal shape. In keratoconus, the cornea is weak with too few cross-links or support beams. This weakened structure allows the cornea to bulge outwards.
The cross-linking procedure adds cross-links or ”cross beams” to the cornea, making it more stable, holding its shape and focusing power better. These new cross-links help strengthen the cornea which can stop the thinning process and further loss of vision.
Can CXL be performed for everyone with keratoconus?
CXL candidates are at least 12 years old and have corneas that are not too thinned or too scarred for the procedure. During your consultation, we will determine if CXL might an option for you. Our practice offers a complimentary, no-touch, painless screening test to see whether CXL might help you.
Should your relatives be tested?
As you may know, keratoconus is a condition that often runs in families, so it’s important to arrange a screening for all family members of patients with keratoconus. If caught early, there is a good chance that CXL can halt the progression of keratoconus and prevent the need for uncomfortable contact lens wear and/or corneal transplant.
How effective is CXL?
Many research studies have shown that CXL may prevent further vision loss in over 95% of patients and improves vision in 60-81% of patients treated.
Is CXL like LASIK?
No. LASIK is a procedure that reduces or, in some cases, may even eliminate the need for glasses or contact lenses by removing corneal tissue. The CXL treatment does not remove tissue.
The purpose of CXL is to prevent further deterioration of vision for patients with corneal conditions such as keratoconus and pellucid marginal degeneration. Some patients may require a lower eyeglass prescription or have an easier time being fit with contact lenses following CXL.
Can CXL prevent the need for a corneal transplant?
Many studies have shown that CXL can often prevent the need for a corneal transplant and allow patients to wear contact lenses or glasses more comfortably and safely again.
Can a corneal transplant be done after CXL?
If CXL does not prevent the need for a corneal transplant, then a corneal transplant can generally be performed. For patients who have already had a corneal transplant, it is still possible to undergo CXL if concerns about stability arise.
What’s the difference between a corneal transplant and CXL?
CXL is an in-office procedure that does not involve surgical incisions into the eye or stitches. It is a relatively non-invasive procedure that is done with vitamin drops and ultraviolet light. Corneal transplants are performed in an operating room, involving incisions into the eye and a lifelong risk of rejection of the corneal tissue.
How long does CXL treatment last?
Based on CXL study results over more than a decade, the beneficial effects of CXL appear to last for many years and there is evidence that this strengthening effect may be permanent.
Is CXL new?
Corneal collagen cross-linking has been performed since 1999. The results and safety profile of CXL have been very positive in numerous studies throughout the world. In fact, by September of 2006, CXL had been approved by all 25 European Union nations. CXL procedures are now routinely performed on patients as young as 10 years old in Europe to prevent the development of keratoconus.
Does CXL need to be repeated?
In many studies, the majority of patients responded to a single vitamin and light CXL treatment and did not need to have the procedure repeated. CXL can typically be repeated if the initial treatment is not effective.
How is CXL performed?
The CXL treatment is an outpatient procedure performed in the doctor’s office using only numbing eye drops and a mild sedative like a Valium tablet. You’ll need to lie flat on your back in a reclining chair and look up at a soft blue light during the treatment.
In the original version of CXL, the epithelium, a thin layer of clear, protective tissue (like skin) that covers the cornea is removed for the CXL procedure. Next, vitamin eye drops (riboflavin) are used in the eye and you will be asked to look at a special blue (ultraviolet) light while lying comfortably on a reclining chair. It’s generally easy to look at this light because your eyes are numb and we use drops so that your eyes won’t feel dry.
What is the transepithelial (or epi-on) CXL technique?
In this less invasive CXL treatment, the surface skin layer (epithelium) of the cornea is not removed so the recovery (visual and comfort) is much faster than the traditional CXL technique. This less invasive technique can only be done on corneas that are thicker than 400 microns. Your surgeon will be able to determine if you might be a candidate for transepithelial CXL treatment.
How long does the procedure take?
If two eyes are being treated at once, the procedure takes approximately an hour and a half. If only one eye is being treated at a time, the procedure takes approximately one hour. Much of the time is spent getting the eye(s) nicely bathed in the vitamin eye drops. The actual UV light treatment time is only about 10 minutes per eye.
Does the CXL procedure hurt?
No. The cross-linking procedure is painless. Anesthetic eye drops are used to avoid any discomfort during the procedure. Some patients have some discomfort after the procedure, and your surgeon can tell you whether you are likely to experience post-procedural discomfort.
Can I have one eye treated at a time?
Yes, and your doctor will discuss the advantages and disadvantages of treating one eye or two eyes at a time.
When is the best time to have CXL?
As with most conditions, prevention of a problem is better than the treatment of a problem. The best time to treat keratoconus is before astigmatism has become severe and vision has been lost. This does not mean that people with very poor vision from keratoconus cannot be helped by CXL. However, the results of CXL for patients with advanced keratoconus have not been as good as for patients with early disease.
If CXL works for me and stops my vision from getting worse, can I have laser vision correction or Intacs afterward?
Some patients may be able to have an excimer laser treatment (PRK) or Intacs to improve their vision without glasses after they have healed from the CXL procedure. Other patients may be able to undergo PRK or Intacs during (or within days of) their CXL procedure.
Do I have to stop wearing contacts before having CXL?
We recommend that you stay out of contact lenses for a week or two if possible before your consultation visit to see if you might benefit from the investigational CXL procedure. This can vary based on how difficult it is for you to see without your contacts. We often suggest patients not wear their lenses for 3 days before their CXL procedure.
Do I have to stop wearing contacts before having CXL?
We recommend that you stay out of contact lenses for a week or two if possible before your consultation visit to see if you might benefit from the CXL procedure. This can vary based on how difficult it is for you to see without your contacts. We often suggest patients not wear their lenses for 3 days before their CXL procedure.
When can I resume wearing contact lenses?
Most patients can return to wearing contact lenses 2 to 6 weeks after having the cross-linking procedure depending on whether you are a candidate for transepithelial CXL. Your surgeon will determine how long this might take in your case.
Will I need new glasses or contacts after CXL?
Because cross-linking can improve vision, patients may find that their old contacts or glasses are too strong for them, and they need to be refit with new glasses and/or contact lenses. Most of the time, patients can wear their old glasses until several months after the procedure at which time their doctor will prescribe new ones. Because the effects of CXL occur slowly, patients don’t generally have to change their glasses very often.
When will I notice any improvement in my vision after CXL?
With the traditional CXL procedure, most patients find that immediately after the cross-linking treatment their vision is actually worse than it was before the procedure. This usually goes on for roughly 3-6 weeks. Patients may start to notice positive effects 4-8 weeks after the procedure and may experience a major improvement in vision 3-6 months later.
In some studies, patients’ vision and astigmatism were still continuing to improve five years after the cross-linking procedure, so visual improvement is a long process. With the less invasive transepithelial CXL, some patients found their vision improved as early as several weeks after treatment. Despite these potential vision improvements, it’s important to remember that the primary reason for considering CXL is the desire to protect against corneal instability and vision loss.
When can I exercise and return to my usual activities after CXL?
We want to help you be able to work or do other things you need and want to do as quickly as possible. Based on the type of CXL procedure, your doctor can tell you when you can reasonably expect to return to your usual activities. With traditional CXL, most people can usually do so after 5-7 days. With transepithelial CXL, most people return to their usual activities the next day.
Does insurance cover CXL treatment?
Depending on your insurance and the type of CXL procedure being performed, it is possible that the procedure will be covered by your insurance. Financing is available to help patients pay for CXL. To find out more about costs, please ask our surgical coordinator.
For more information about keratoconus, and/or our diagnostic screenings and treatments, please call our practice and ask to speak with a CXL coordinator or visit our website.



